King's Fellow Ashley Moffett and her laboratory have been involved with a ground-breaking project to grow “mini placentas” that could transform research into the underlying causes of miscarriage, stillbirth and other pregnancy disorders.
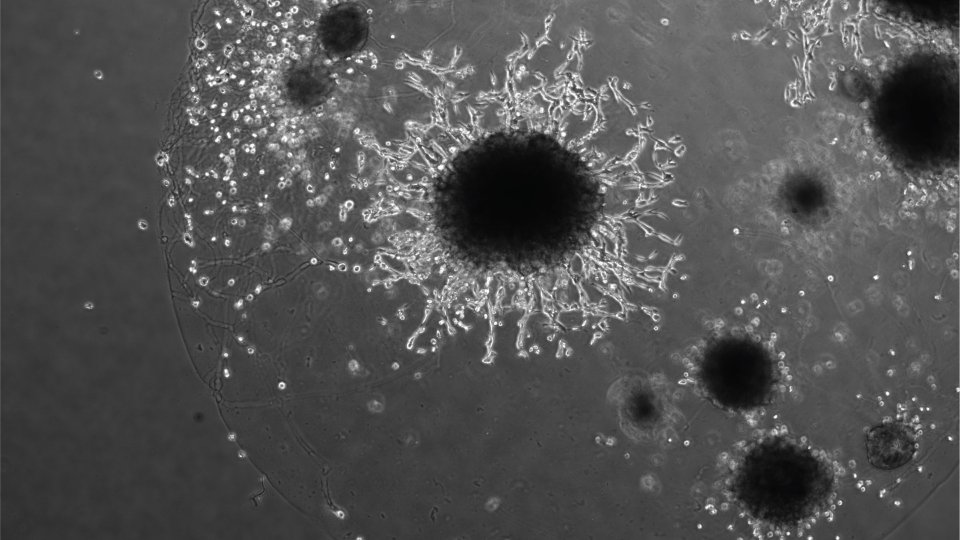
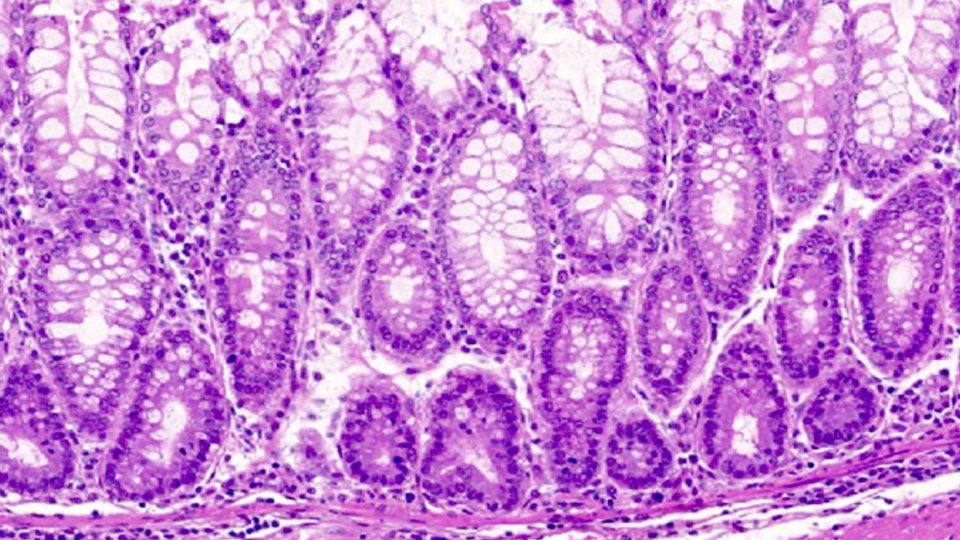
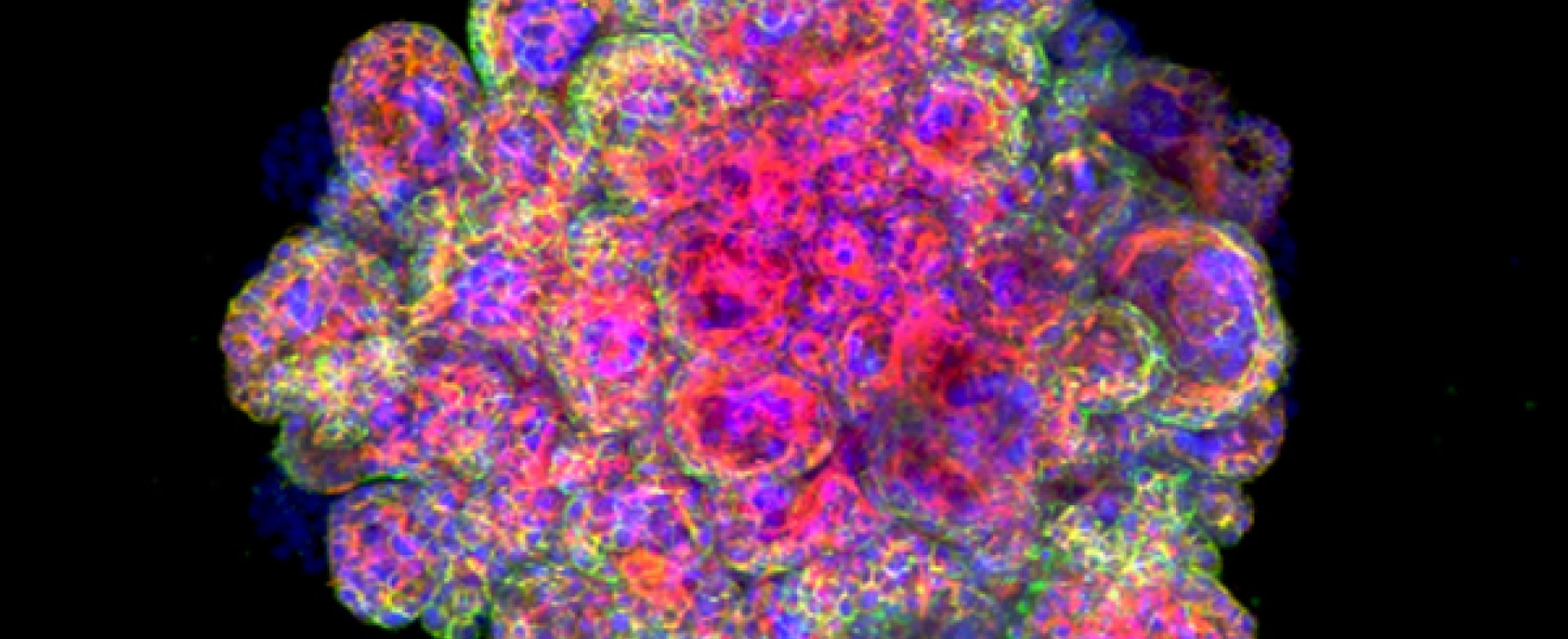
In a study funded by the Centre for Trophoblast Research and the Wellcome Trust, Professor Moffett's team was able to grow organoids using cells from villi – tiny frond-like structures – taken from placental tissue. These trophoblast organoids are able to survive long-term, are genetically stable and organise into villous-like structures that secrete essential proteins and hormones that would affect the mother’s metabolism during the pregnancy. Further analysis showed that the organoids closely resemble normal first-trimester placentas. In fact, the organoids so closely model the early placenta that they are able to record a positive response on an over-the-counter pregnancy test.
Efforts to grow human placental cells started over 30 years ago in the Pathology department where Professor Moffett and another King's Fellow, Charlie Loke, were studying cellular events in the first few weeks of pregnancy. With their chief technician, Lucy Gardner, they found ways to isolate and characterise placental trophoblast cells. These techniques, combined with the organoid culture system, enabled the generation of miniature functional models of the early placenta – or ‘mini-placentas’. In the past few years, a new field of research has blossomed that uses these organoids – often referred to as ‘mini-organs’ – enabling insights into human biology and disease.
The creation of these mini-placentas may help explain cases where the embryo does not implant correctly into the lining of the womb (uterus) and fails to form a placental attachment to the mother. Because of the complexities of studying this early period of our development, very little is understood about what is happening normally and what can go wrong, and other animals are too dissimilar to humans to provide a good model of placental development and implantation.
Professor Graham Burton, a co-author and Director of the Centre for Trophoblast Research, which last year celebrated its tenth anniversary, said:
“These ‘mini-placentas’ build on decades of research and we believe they will transform work in this field. They will play an important role in helping us investigate events that happen during the earliest stages of pregnancy and yet have profound consequences for the life-long health of the mother and her offspring. The placenta supplies all the oxygen and nutrients essential for growth of the fetus, and if it fails to develop properly the pregnancy can sadly end with a low birthweight baby or even a stillbirth.”
In addition, the organoids may shed light on other mysteries surrounding the relationships between the placenta, the uterus and the fetus: why, for example, is the placenta able to prevent some infections passing from the mother’s blood to the fetus while others, such as Zika virus, are able to pass through this barrier? The organoids may also be used for screening the safety of drugs to be used in early pregnancy, to understand how chromosomal abnormalities may perturb normal development, and possibly even provide stem cell therapies for failing pregnancies.
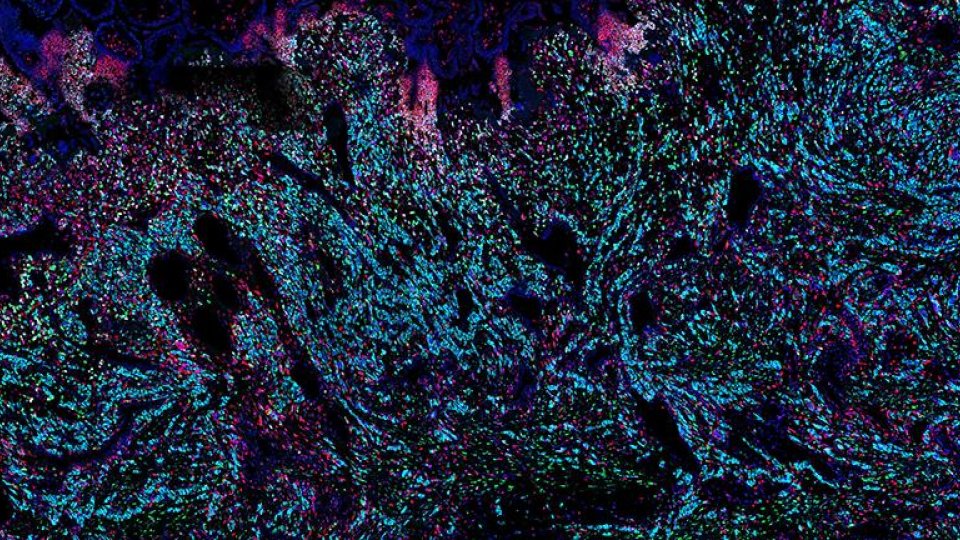
Professor Moffett also co-directed a recent study published in Nature that used genomics and bioinformatics approaches to map over 70,000 single cells at the junction of the uterus and placenta. This study revealed how the cells talk to each other to modify the immune response and enable the pregnancy, presenting new and unexpected cell states in the uterus and placenta, and showing which genes are switched on in each cell.